While we typically think of altitude as a stimulus to make our training harder, and get more bang for buck from your session, in recent years we’ve witnessed a new trend in implementation: injury rehab. It’s something that’s been led by the clubs we work with in the Premier League and is increasing in its popularity in elite sport and with recreational athletes looking to get back to sport sooner. Performance Specialist, Maisie Rose, takes a look at the science behind altitude in rehab…
Hypoxia plays an important role in promoting healing across various types of tissue by activating key biological pathways that are essential for regeneration. These pathways include angiogenesis (formation of new blood vessels), osteogenesis (formation of new bone) and the growth and repair of damaged tissues.
Hypoxia-Inducible Factor 1-alpha (HIF1-a)
To truly understand the benefits of utilising hypoxia for injury rehabilitation, we need to look at and understand all the factors which are stimulated by a hypoxic environment. The first, and arguably most important, is HIF1-a. HIF1-a is a transcription factor that detects low oxygen levels in the blood and triggers a series of responses. It upregulates the transcription of certain genes which improve oxygen delivery to tissues, promoting healing, and supporting tissue repair.
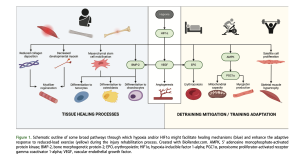
Angiogenesis
Arguably the most important downstream target of HIF1-a is the vascular endothelial growth factor (VEGF). VEGF is a protein which promotes angiogenesis, the production of new blood vessels from existing blood vessels. By promoting angiogenesis, VEGF increases blood supply to the injured area meaning an increased delivery of oxygen and removal of waste products, which in turn accelerates the healing process.
Adenosine Monophosphate-activated Protein Kinase (AMPK-a )
HIF1-a also stimulates production of a protein called adenosine monophosphate-activated protein kinase (AMPK-a) which plays a crucial role in muscle tissue repair and regeneration. AMPK-a has a few roles and tries to keep things running smoothly by coordinating responses to stress, such as hypoxia. For example, it stimulates the activation and proliferation (increase) of satellite cells, specialised stem cells responsible for muscle regeneration. These cells multiply, mature and fuse together to rebuild muscle fibres. AMPK-a also helps clear out damaged cellular components via autophagy and keeps energy use efficient by inhibiting energy hungry pathways which are not required during recovery. This rerouting ensures resources are focused on recovery rather than unnecessary pathways during stress. This highlights the use of hypoxia enhancing rehabilitation, not just by accelerating tissue repair but also by fine-tuning energy use. AMPK-α overexpression in hypoxia-treated rats suggests this molecular pathway enhances muscle tissue repair.
Implementing Hypoxic Exposure
Here on site, we implement hypoxic exposure in the form of Intermittent Hypoxic Exposure (IHE) achieved via our MetraFit PODs. If you have a big event coming up and have been set back by an unexpected injury, the use of IHE can help to speed up your recovery process. We all know how frustrating it can be to have an injury when we want to train, but what if you could put your feet up and destress knowing the hard-earned fitness will last another day.
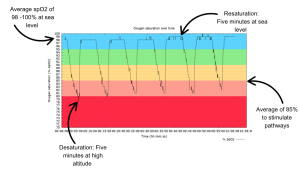
IHE involves breathing at high altitude while at rest. You receive five minutes of high-altitude air though a mask, followed by five minutes at sea level (see Figure 2). This allows your blood oxygen saturation (spO2) to drop from where it is at sea level (98-100%) to around 80% during the five minutes at high altitude. The aim of the session is to achieve an average spO2 of 85% across the hour (see Figure 2). This intermittent exposure can help stimulate your body’s natural repair mechanisms by activating the processes outlined above, and ultimately speed up recovery. This is an incredibly powerful tool for athletes who are desperately trying to avoid large levels of reversibility when coming back from an injury.
Case Study Bones: A Cyclists Journey to Recovery
Let’s take a look at the real-world application of hypoxia in injury rehabilitation. A cyclist, who joined us at the centre after having broken his thumb whilst training for a ride through the Dolomites. He was desperate to return to the bike and was looking for a way to speed up his return in order to make his trip.
When he joined the centre, we started him on a course of IHE to support and accelerate his bone healing. The reason for this is that research shows IHE activates HIF1-a, which in turn promotes blood vessel formation, encourages bone regeneration and boosts woven bone density around the injured site. Research surrounding this topic highlights that Bone Morphogenetic Proteins (BMPs), which regulate bone formation, and the differentiation of Mesenchymal Stem Cells (MSCs) into osteogenic and chondrogenic cells (forms new cartilage) are also enhanced in hypoxic conditions. Research has shown that the use of IHE can significantly improve bone minderal density (Camacho-Cardenosa et al., 2020). Essentially, IHE serves as a catalyst for optimising healing and offering a more efficient recovery process for patients suffering from bone injuries, potentially reducing recovery times and improving long-term outcomes. A combination of all these factors allowed his thumb to heal faster than expected. The upshot was that he made a good recovery from the broken thumb and was able to make the Dolomites trip and despite being off the bike for around 6 weeks, this strongly showcases the power of hypoxia in bone recovery.
Why IHE?
Lots of people ask why IHE, why not a continuous hypoxic exposure? (Chronic hypoxia). There is research to support both the use of IHE and suggest that people should avoid chronic hypoxia when it comes to injury rehabilitation. Behrendt et al., 2022 found intermittent hypoxic exposure protocols may have a role in tissue repair and recovery. Research has found that chronic hypoxia may actually have a negative impact on muscle healing, by inhibiting satellite cell activity resulting in delayed muscle fibre formation and growth (Chaillou et al., 2014) and the delayed differentiation into certain bone cells (Camacho-Cardenosa et al., 2020). Here at the centre, we have found that 2-3 sessions of IHE per week of for six weeks is optimal for athletes looking to accelerate their recovery from muscle injuries.
Case Study Ligaments & Tendons: Lions Rugby Player
However, bone recovery is just one aspect of healing in the body and IHE is only one method that we can use in injury rehab. Ligaments (which connect bone to bone) and tendons (which connect muscle to bone) can both be slow to heal if damaged as they receive a very limited blood supply. This means that, unlike muscles, which have a richer vascular network, ligaments and tendons receive less oxygen and fewer nutrients which can mean that healing is a slow process.
Let’s take a look at another example of an athlete we have worked closely with for injury rehabilitation. A player who had been selected for the British and Irish Lions tour to South Africa suddenly dislocated a shoulder less than 3 weeks out from the start of the tour. To aid his recovery, and retain his cardiovascular fitness, his sport science team instantly had him use an altitude tent. By sleeping at altitude, the player was able to maximise his exposure to hypoxia, which was important in his recovery. This is because the hypoxic environment in the tent helped promote the differentiation of MSCs differentiation into tenocytes and the upregulation of the scleraxis gene which aids tendon repair and regeneration. In term of his cardiovascular fitness, HIF1-a also promotes erythropoietin (EPO) synthesis (Haase, 2010). EPO is essential in red blood cell production which is important in maintaining cardiovascular health as more red blood cells mean more oxygen transport around the body.
So, whether you are dealing with tendonitis or a more severe tendon injury, incorporating Hypoxic exposures into your recovery routine could significantly accelerate the healing process.
Conclusion
Although much of the research on hypoxia and injury rehabilitation has been conducted using animal models, the results are promising. Ethical considerations and the complexities of human trials make it difficult to conduct similar studies in humans, but we continue to see significant improvements in injured athletes using hypoxia-based rehabilitation here on site. From cyclists to rugby players, the benefits of hypoxia in speeding up recovery and enhancing performance are evident, and we are excited to continue making a difference.
In conclusion, whether you’re dealing with a broken bone, tendonitis, or muscle strain, hypoxia-induced healing offers a powerful tool for faster and more effective rehabilitation. By understanding and harnessing the power of IHE, we can help the body recover faster so that you are back on your feet in no time.
What Now? Book onto…
References:
Behrendt, T., Bielitzki, R., Behrens, M., Herold, F. and Schega, L., 2022. Effects of Intermittent Hypoxia–Hyperoxia on Performance- and Health-Related Outcomes in Humans: A Systematic Review [Online]. Sports Medicine – Open, 8(1). Available from: https://doi.org/10.1186/s40798-022-00450-x [Accessed 30 October 2022].
Chaillou, T., Koulmann, N., Meunier, A., Pugnière, P., McCarthy, J.J., Beaudry, M. and Bigard, X., 2014. Ambient hypoxia enhances the loss of muscle mass after extensive injury [Online]. Pflugers Archiv : European journal of physiology, 466(3). Available from: https://doi.org/10.10 07/s00424-013-1336-7 [Accessed 27 October 2022].
Camacho-Cardenosa, M., José Manuel Quesada-Gómez, Camacho-Cardenosa, A., Leal, A., Dorado, G., Bárbara Torrecillas-Baena and Casado-Díaz, A., 2020. Effects of normobaric cyclic hypoxia exposure on mesenchymal stem-cell differentiation–pilot study on bone parameters in elderly [Online]. World Journal of Stem Cells, 12(12), pp.1667–1690. Available from: https://doi.org/10.4252/wjsc.v12.i12.1667 [Accessed 30 January 2025].
Haase, V.H., 2010. Hypoxic regulation of erythropoiesis and iron metabolism [Online]. American Journal of Physiology – Renal Physiology, 299(1), pp.F1–F13. Available from: https://doi.org/10.1152/ajprenal.00174.2010 [Accessed 27 March 2020].

